CMS recently published the CY 2023 Quality Payment Program (QPP) Proposed Rule which included numerous proposed updates to MIPS Value Pathways (MVPs) and Merit-based Incentive Payment System (MIPS). For the full text of the rule, see the Federal Register.
MIPS Value Pathways (MVPs)
CMS is continuing to move to MIPS Value Pathways (MVPs) to “improve value, reduce burden, inform patient choice in selecting clinicians, and reduce barriers to participation in Alternative Payment Models (APMs).” To that end, CMS is proposing 5 new MVPs and revising the 7 previously established MVPs that would be available beginning with the 2023 performance year.
The 5 newly proposed MVPs for the 2023 performance year are:
- Advancing Cancer Care
- Optimal Care for Kidney Health
- Optimal Care for Patients with Episodic Neurological Conditions
- Supportive Care for Neurodegenerative Conditions
- Promoting Wellness
CMS also made proposals for subgroup reporting to MVPs. While CMS previously finalized that a subgroup must provide a list of TIN/NPIs in the subgroup and a plain language name for the subgroup during registration, CMS is also proposing that subgroups include a description of the composition of the subgroup. Further, CMS is proposing that subgroups would be assigned the affiliated group’s score for the Foundational Layer measure, outcome-based administrative claims measures in the Quality category, and the Cost performance category. If a group score is not available, then the measure will be excluded from the subgroup’s final score. Lastly, for subgroups that register but don’t submit data as a subgroup, CMS is proposing to not assign a score.
Traditional MIPS
For 2023 MIPS reporting, the MIPS score will continue to be based on the four performance categories and their corresponding weights. CMS is proposing the performance threshold will not change for 2023 performance period and remain at 75 points. The 2022 performance year was the final year for additional MIPS adjustment for exceptional performance.
Quality
For the Quality category, CMS is proposing a total of 194 measures for the 2023 performance period. CMS is proposing the addition of 9 quality measures, including 1 new administrative claims measure, 1 composite measure, 5 high priority measures, and 2 new patient-reported outcome measures.
CMS is proposing that administrative claims measures will be scored using performance period benchmarks, while quality measures will continue to be scored using historical benchmarks.
For the 2024 and 2025 performance periods, CMS is proposing to increase data completeness to 75%.
Cost
Beginning with the 2022 performance period, CMS is proposing to establish a maximum cost improvement score of 1 percentage point out of 100 percentage points available for the cost performance category.
Improvement Activities
CMS is proposing to update the improvement activities inventory by adding 4 new improvement activities, modifying 5, and removing 6.
Promoting Interoperability
Beginning with the 2023 performance period, CMS is proposing to discontinue automatic reweighting of the Promoting Interoperability (PI) category for nurse practitioners, physician assistants, certified registered nurse anesthetists, and clinical nurse specialists.
CMS is proposing to allow APM Entities to report PI data at the APM Entity Level when participating in MIPS at the APM Entity level. This is a change to how APM Entities had to report PI data at the individual or group level.
Currently the Public Health and Clinical Data Exchange Objective includes 3 levels of active engagement. CMS is proposing to reduce the levels of engagement to 2 by combining Options 1 and 2 into a single option titled, “Pre-production and Validation” and rename option 3 to “Validated Data Production.” In addition to requiring a yes/no attestation for the required measures under this objective, CMS is proposing to require the submission of level of active engagement. CMS is also proposing that MIPS eligible clinicians may only spend one performance period at the Pre-production and Validation level of active engagement per measure and they must progress to Validated Data Production level in the next performance period for that particular measure.
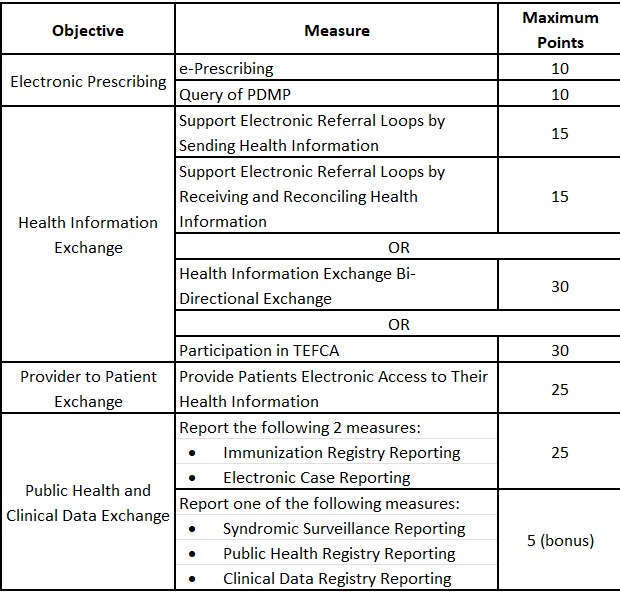
The Query of the Prescription Drug Monitoring Program (PDMP) has been an optional measure for bonus points, but CMS is proposing to make it required beginning with the 2023 performance period worth 10 points, with exclusions available. The proposal also includes expanding the scope of the measure to not only include Schedule II but also Schedules III and IV drugs.
CMS is proposing a 3rd option for the HIE Objective for the 2023 performance period, Participation in the Trusted Exchange Framework and Common Agreement (TEFCA). MIPS Eligible clinicians would be required to attest Yes to being a signatory to a Framework Agreement as that term is defined by the Common Agreement for Nationwide Health Information Interoperability as published in the Federal Register and on the Office of the National Coordinator for Health Information Technology (ONC) website and use CEHRT to exchange information under this Agreement.
Beginning with 2023 performance period, CMS is proposing the following maximum points for the PI measures:
If you have questions about MIPS/MVPs reporting, please contact us.

